The World Health Organization (WHO) declared mpox a global public health emergency on Aug. 14 following an upsurge of cases in Congo and African countries. It warned against the potential spread of the disease outside the continent and called for a coordinated international response to stop the outbreak.
While the Department of Health (DOH) has acknowledged the urgency of WHO’s declaration, it assured the public that mpox differs from the COVID-19 pandemic and advised them to remain alert.
“Tamang praning lang, ‘wag masyado kasi para alam din natin kung ano ang gagawin natin para ‘di tayo mahawahan o tayo ay makapag-ingat,” Health Spokesperson Albert Domingo said on Aug. 15. (Don’t be too paranoid, so we’ll know how to avoid getting infected or be cautious.)
The DOH confirmed on Sept. 1 that three new patients were diagnosed with mpox from Metro Manila and CALABARZON. This brings the total number of mpox cases in the country since July 2022 to 17: nine have recovered while eight are active cases diagnosed this year.
Here are five things you need to know about the latest public health emergency:
1. What is mpox?
Mpox is an infectious zoonotic disease caused by the “monkeypox virus” belonging to the same family that causes smallpox. It is regularly found among small rodents, monkeys and other mammals in Central and West Africa but is occasionally passed on to people, resulting in small outbreaks.
The monkeypox virus has two types: clade I and clade II. Clade I is associated with more severe symptoms and deaths. The spread of its subtype Clade Ib prompted WHO to sound its top emergency alarm.
Clade II caused the global outbreak that began in 2022 and is considered less severe. This is the type that is currently spreading in the Philippines.
On Aug. 21, Health Secretary Teodoro Herbosa explained that mpox is a DNA virus that mutates at a much slower rate, unlike RNA viruses such as COVID-19 which mutate rapidly, causing more variants.
The WHO renamed the disease from monkeypox to mpox in 2022 to follow modern guidelines for naming illnesses. The guidelines recommend the scientific community to avoid using names that may “offend cultural, social, national, regional, professional or ethnic groups” and to “minimize unnecessary negative effects on trade, travel, tourism or animal welfare.”
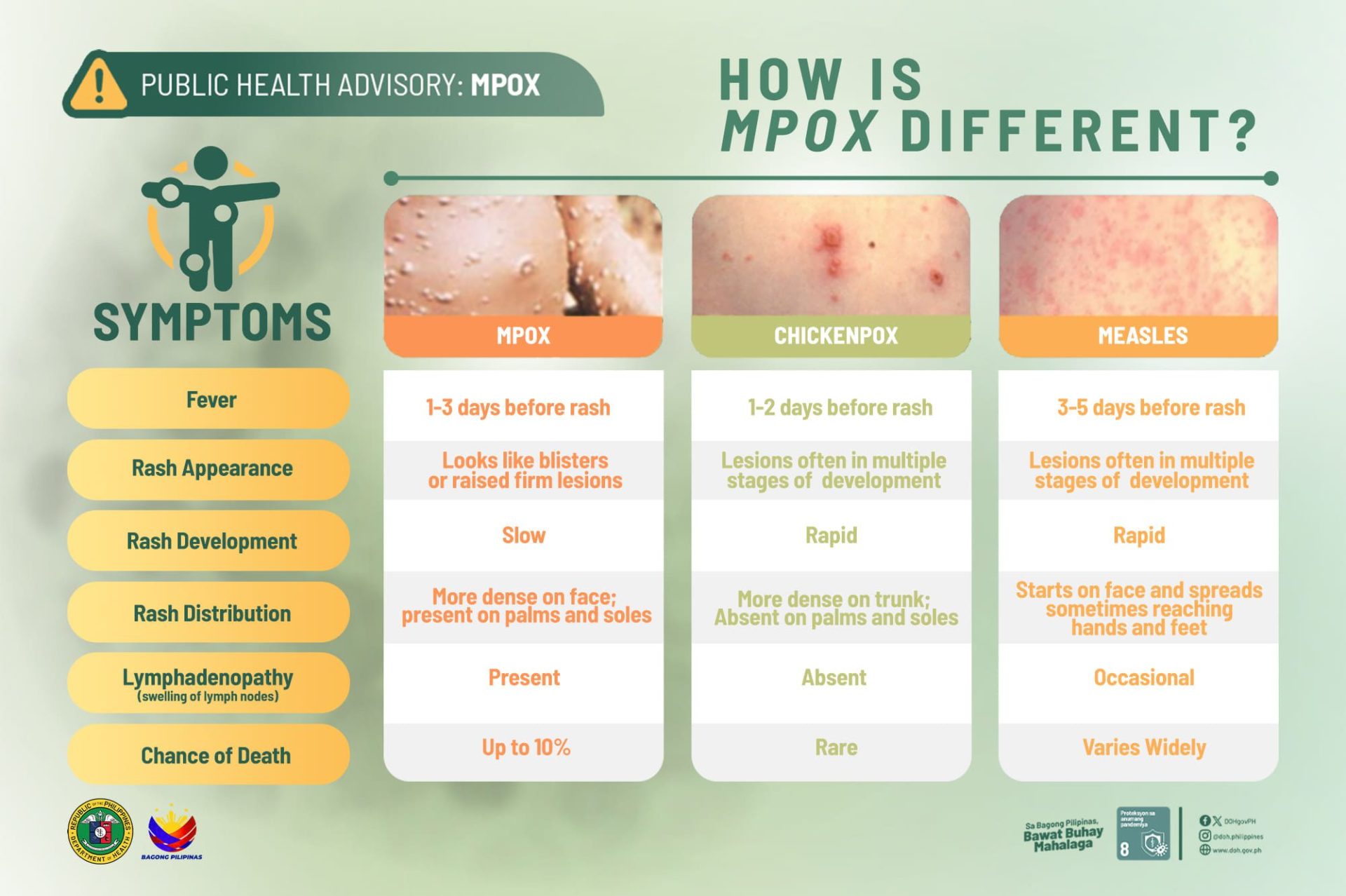
2. What are the symptoms of mpox?
Common symptoms of mpox include rashes, fever, sore throat, headache, muscle aches, back pain, low energy and/or swollen lymph nodes.
The rashes caused by mpox often begin showing up on the face and later spread over the body, up to the palms of the hands and soles of the feet. They undergo various stages, including scabs, before healing.
Symptoms typically show up within a week of contracting the virus but may manifest anywhere from one to 21 days after exposure.
3. How does it spread?
According to WHO, the disease can spread from one person to another mainly through close contact with someone who has mpox. It can be passed on “until all sores have healed and a new layer of skin has formed.”
Close contact includes skin-to-skin, mouth-to-mouth and mouth-to-skin such as touching, kissing and sexual intercourse.
The disease can be transmitted from an infected animal to a person through bites, scratches or when people hunt and eat them. The virus can also spread through respiratory droplets or contact with a contaminated object.
4. How is mpox treated and what to do when infected?
The goal in treating mpox is to take care of the rashes, manage pain and prevent complications, the WHO said. Those infected by the disease can typically recover within two to four weeks.
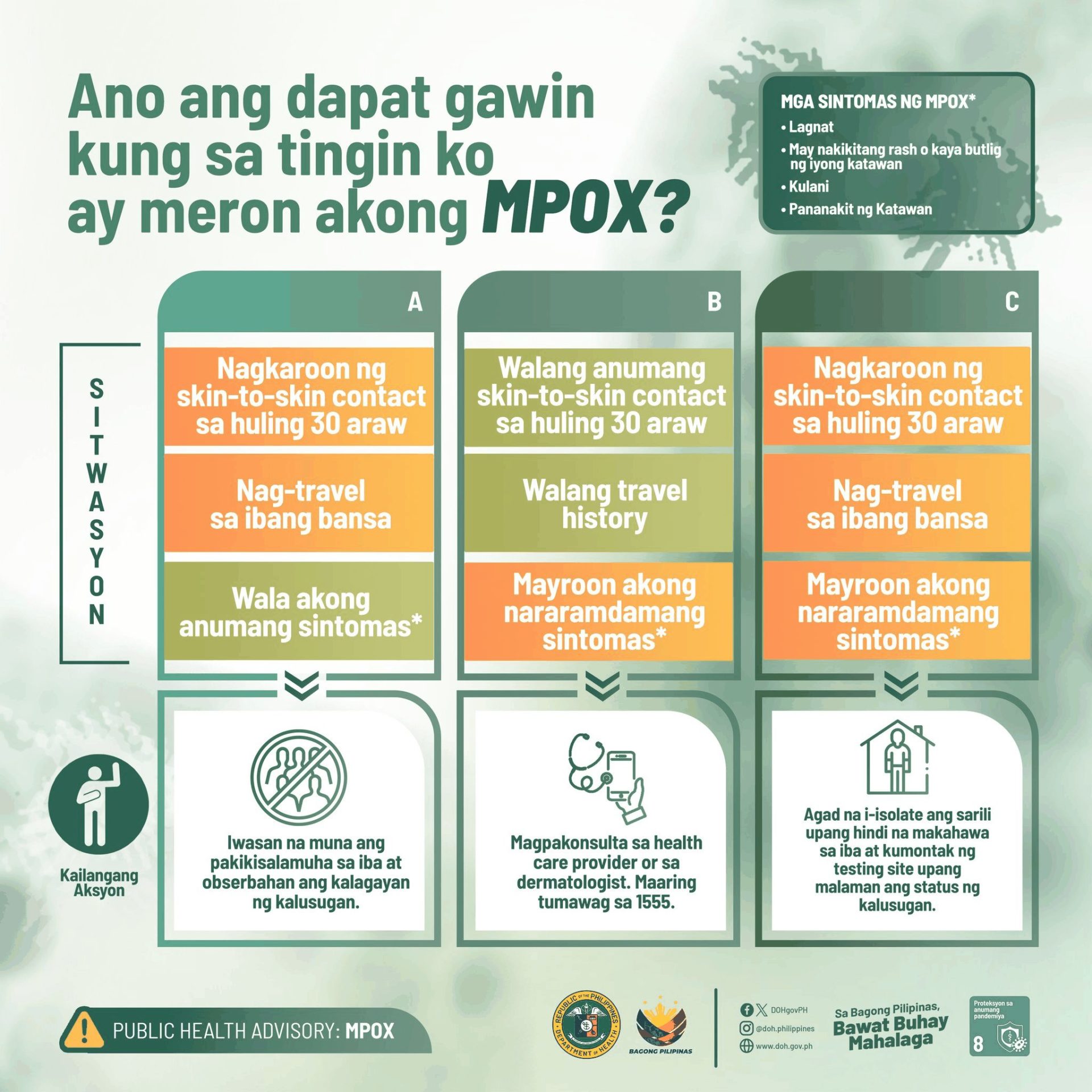
Depending on their situation, travel history and symptoms experienced, persons suspected to have the disease are advised to self-isolate, contact a healthcare provider and/or contact a testing site.
Current testing sites for mpox include: Research Institute for Tropical Medicine, San Lazaro Hospital, East Avenue Medical Center, Jose Reyes Memorial Medical Center, Jose N. Rodriguez Memorial Hospital (Tala Hospital), Quirino Memorial Medical Center and UP – Philippine General Hospital.
5. How to prevent the disease?
According to the United States Centers for Disease Control and Prevention, multiple ways exist to protect oneself from getting mpox. These include:
- avoiding close, skin-to-skin contact with people who have rashes that look like mpox and with infected animals;
- learning how to lower your risk of mpox during sex or at a social gathering; and
- getting vaccinated.
The DOH reminded the public to “consistently adhere” to health protocols, particularly observing respiratory etiquette (wearing masks or covering your mouth when coughing or sneezing), ensuring good airflow and washing hands frequently with soap and water or alcohol-based hand sanitizer.
It further cautioned people to avoid contact with animals possibly carrying mpox. This includes sick or deceased animals found in areas where the disease is present.
Get more insights:
Ask SEEK
Have you seen any dubious claims, photos, memes, or online posts that you want us to verify? Fill out this reader request form or send it to VERA, the truth bot on Viber.
(Guided by the code of principles of the International Fact-Checking Network at Poynter, VERA Files tracks the false claims, flip-flops, misleading statements of public officials and figures, and debunks them with factual evidence. Find out more about this initiative and our methodology.)
